July 8, 2010
New medical interns express enthusiasm, get pointers from veterans
Drink coffee. Go to the dentist. Don’t drive home after you’ve been on call. Page your senior resident and others more often, rather than less. Help each other out. Write everything down.
New medical interns heard these words of wisdom on Thursday, June 24, from older residents at the UW. Interns, as they’re called, have completed medical school. The internship lasts one year and after that time, many of the doctors will head off to finish graduate medical education in a specialty track.
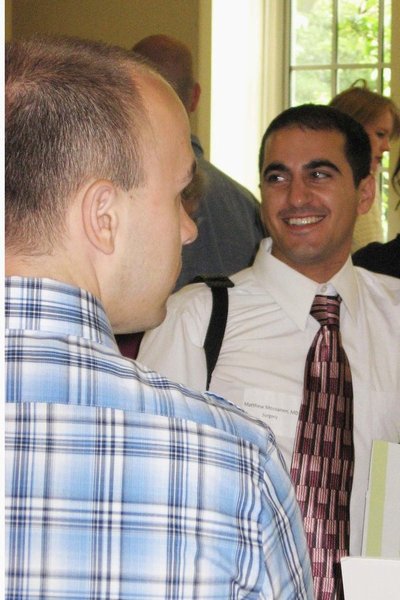
Dr. Matthew Mossanen, who hails from Los Angeles, recently graduated from UCLA. He’ll spend an intern year in general surgery and, afterwards, will specialize in urology. He chose the UW School of Medicine and Seattle for many reasons, including the unique and diverse health care systems that exist. “Academically, the UW is tip-top,” Mossanen said. “Seattle is a wonderful city, the research at the UW is very strong and faculty are tremendously friendly.” He looks forward to learning how to take care of patients. “It’s the biggest challenge, but also the most exciting.”
Fellow surgical interns — and recent UW School of Medicine grads — Laura Stoll and Kathleen Berfield also expressed enthusiasm about what lies ahead. How does it feel to have an official “M.D.” after their names? “It’s hasn’t really sunk in yet,” said Stoll, with a smile. Berfield said it feels a little surreal.
Stoll will specialize in orthopedic surgery, while Berfield will become a cardiothoracic surgeon — the first resident to do so in a newly-created program. “Initially, I came in thinking I would choose family medicine,” said Berfield. “But I loved surgery rotations and had the greatest time,” she said, beaming with authentic pride. Lungs are so cool and neat, she said, in a way others might describe an interesting painting or a cute outfit. “It sounds totally dorky, but being able to touch a beating heart, it’s incredible,” Berfield said.
Resident program directors are used to that kind of enthusiasm. They also must have a similar level of good cheer, given that the director role — on top of the day job — adds up to loads of extra work. Dr. Doug Hanel, UW professor in orthopaedics and sports medicine, said that he initially sorts through 600 applications to fill eight positions. More than 60 doctors come to Seattle for interviews and the proverbial “best of the best” are chosen for the UW program. “We’re exceedingly lucky because our applicants represent the top 10 percent of their medical school classes,” said Hanel. The doctors’ board scores are routinely above the 75th percentile, too, and incoming interns arrive with honors from medical and surgical rotations.
Half of the orthopedic residents are women this year. But Hanel said that did not happen because of any type of mandate or special look. “We pursue candidates based on the strength of their applications,” he said.
Dr. Richard Shugerman, UW professor of pediatrics based at Seattle Children’s, has an equally large workload as residency program director. Applications number 1,000 for some 33 spots, he said. About 750 of those applications are from within the United States. Across the country, approximately 1,700 U.S. medical students (40 percent of the entire pool) each year choose to go into pediatrics.
Interview “season,” as he called it, runs from mid-October to mid-January. Up to 300 applicants may be invited to Seattle for interviews and residents play a very active role, said Shugerman. Faculty and residents — a 50/50 split — comprise the final selection committee. “Everybody reads all the files of everyone who’s been interviewed, makes a rank list and then we average our rank list. That’s how we determine who we want to rank on our list. It gets our residents really involved, gives them a real sense of ownership and gives us a great group of interns.”
Shugerman said residency selection is truly a time-intensive process (with three interviews per week over three months), but also well worth the investment. “Two-thirds of our residents end up staying in the WWAMI region for fellowships or to go into practice,” he said. “We’re helping to choose people who will be the face of pediatrics in the region, so we think it’s worth it.” (The UW is the only civilian pediatric residency program in the WWAMI region. Madigan Army Medical Center has a small program.)
In recent years, Shugerman said that he and his team have worked hard to increase diversity and minority recruitment in the program. Armed with a grant from the UW, the program launched a visiting rotation for fourth year medical students. “We offer under-represented minorities an opportunity to do a rotation at UW in pediatrics,” said Shugerman. The UW pays travel costs and arranges housing, providing minority students with a look at Seattle Children’s, the UW and Seattle in general.
The number of minority student applications has already increased from 42 in 2006 to 62 this year, he said.
New residents at the June orientation also heard about Seattle Children’s perks, as older residents played a friendly game of one-upmanship while sharing advice. “They have the best showers,” said one resident, chuckling.
But the best advice of all, perhaps, was a reminder about the amazing things that doctors, nurses and health-care teams are involved in at medical centers and clinics. “Realize you’re doing cool stuff,” said one resident. “There’s a reason why they have TV shows like Grey’s Anatomy and ER.”