June 23, 2005
Eye surgeon returns to China to implant artificial cornea
Only the size of a button, the tiny plastic disc doesn’t look like much at first glance. But to a person needing a cornea, it can mean the difference between having sight and being blind.
The button, formally called a keratoprosthesis, is an artificial cornea used to restore vision to patients with severely damaged corneas.
In June 2004, Dr. Tueng Shen, Northwest Lions Foundation assistant professor of ophthalmology in the UW School of Medicine, performed the first artificial cornea implant of its kind in the Northwest at UW Medical Center, on a patient from Moses Lake injured on the job.
And in January of this year, Shen traveled to China to perform the first artificial cornea implant in that country.
“The cornea is the clear window at the front of the eye that provides physical protection to the eye and is part of the eye’s focusing power required for sight,” Shen said.
For Hongchuan Zhang, a 23-year-old man from China’s Yunnan Province, like most artificial cornea recipients, the implant was a last resort.
“An artificial cornea is used to restore vision to patients who reject a normal human tissue transplant. For some, like Hongchuan Zhang, an artificial device is just what the doctor ordered. For thousands of people around the world, it represents a new hope to have their vision restored,” Shen said.
Shen was in China on her first volunteer trip for Orbis International, a U.S.-based non-profit organization dedicated to curing and preventing blindness worldwide.
Recruited by Orbis to lead an intensive, one-week training session for the province’s ophthalmologists, Shen led her Chinese colleagues through dozens of sight-restoring operations, during which she demonstrated new surgical techniques.
Zhang had lost vision in both eyes from a chemical burn in July 2004, and had undergone several donor cornea transplants that produced only minor results.
Shen used an artificial cornea implant known as the Boston K-Pro, developed by her mentor at Harvard and the Massachusetts Eye and Ear Infirmary, Dr. Claes Dohlman, and donated for the Orbis mission to China.
“This K-Pro was approved by the FDA in 1992,” Shen said. “It has been implanted approximately 300 times, but mainly in the United States and Europe and never before in China.”
While the full extent of Zhang’s vision recovery will not be known for several more months, he was able to read the clock on the hospital’s wall after only 24 hours, Shen said. His vision has now improved to 20/40.
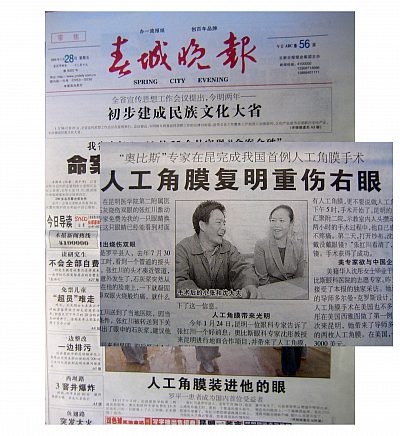
“He told me that with his eyesight restored, he was going to find a new job, a girlfriend and get married,” Shen said with a laugh. The story of Shen and her patient attracted wide attention in the Chinese press and in some Chinese-American publications.
Shen is one of the few doctors in the United States qualified to perform the type of surgery that saved Zhang’s sight. She is director of UW Medical Center’s Refractive Surgery Center and came to the University in 2003.
The trip to China was an emotional one for Shen, who immigrated with her family to the United States from her native city of Shanxi when she was 17. Her father, a biology professor in China, worked in a Chinese restaurant in Boston to support his family.
To learn English, Tueng would stay with a local Boston family on the weekends. She was accepted to Wellesley College, and studied chemistry before receiving a Ph.D in medical engineering from MIT and her medical degree from Harvard Medical School. She also completed her ophthalmology residency at Massachusetts Eye and Ear Infirmary, affiliated with Harvard.
She said she chose ophthalmology as a specialty in part because of how it can literally change people’s lives by restoring their sight.
Shen is focusing her research work in collaboration with Bioengineering Professor Buddy Ratner’s group at the UWEB on developing engineered biomaterials for use with the artificial cornea. Currently donor tissue must be used as a backing for the artificial implant, and it is in limited supply.
“Going back to China, I really saw the magnitude of corneal blindness and the limitations of adequate treatment there. This is a typical challenge in many developing countries. In fact, more than 90 percent of treatable corneal blindness worldwide still remains untreated today.
“This new technology not only changed the outlook on one young life, but also touched many around him, myself included. The challenge is getting expertise and resources to where it is needed the most. I see this as a great opportunity for the development of global medicine,” Shen said.
China faces a huge challenge to reduce avoidable blindness among its 1.3 billion population. An estimated 5.4 million Chinese are blind, including 400,000 children.
“Yunnan province, where Mr. Zhang lives, is among the poorest in China,” Shen said. “It faces a huge task in eliminating avoidable blindness.”
Shen made a second trip to China in mid-June to train another group of physicians there about artificial cornea transplant.