January 28, 2010
Severe complications of diabetes higher in depressed patients
Depression raises risks of advanced and severe complications from diabetes, according to a prospective study of Group Health primary-care patients in western Washington. These complications include kidney failure or blindness, the result of small vessel damage, as well as major vessel problems leading to heart attack or stroke.
The findings were published this week in Diabetes Care, a scientific journal of the American Diabetes Association. The study was conducted by scientists from the Group Health Research Institute, Seattle; the University of Washington (UW) School of Medicine and School of Public Health, and the Veterans Affairs Puget Sound Health Care System. The lead author is Dr. Elizabeth Lin of the Group Health Research Institute.
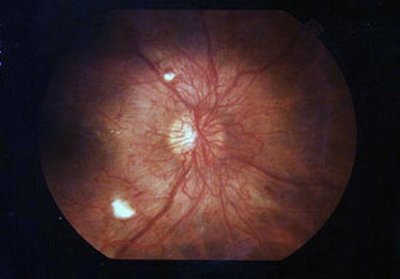
Among their research volunteers with type 2 diabetes followed over 5 years, major depression was associated with a 36 percent higher risk of developing advanced micro-vascular complications, such as end-stage kidney disease or blindness, and a 25 percent higher risk of developing advanced macrovascular complications, such as stroke or myocardial infarction (heart attack from a blood clot), compared with diabetes patients without depression. The clinically significant risks remained even after the researchers adjusted for diabetes severity and self-care activities.
Between 2000 and 2002, the Pathways Epidemiological Follow-up Study enrolled 4,632 primary-care Group Health Cooperative patients with diabetes. These patients were tracked through 2005-2007. The final sample size was 3,922. The researchers reviewed medical records, diagnostic and procedural codes, lists of prescribed medications, and death certificates to determine what happened to each patient over nearly five years. The researchers used proportional hazard models to calculate the association between depression and the risk of advanced complications. Even among patients with diabetes who had no prior indication of microvascular or macrovascular problems, depression increased the chances that these problems would develop.
As in earlier reports, the diabetes patients with major depression tended to be slightly younger, heavier, have more co-existing medical conditions, and were more likely to be treated with insulin than were diabetes patients without depression. They also had higher levels of a substance in the blood formed when the sugar glucose attaches to hemoglobin, an oxygen-carrying protein. The major depression group had a higher proportion of women and smokers. However, after controlling for these differences between depressed and non-depressed patients with diabetes, the increased risk of complications associated with depression remained.
Several previous studies suggest the negative relationship between depression and diabetes cuts both ways. People with depression are prone to diabetes, and vice versa. Impairment from diabetes, such as blindness or kidney failure requiring long-term dialysis, interferes with a person’s daily life and can be overwhelming. The person may become depressed or an existing depression may worsen.
As the incidence of type 2 diabetes soars, the clinical and public health significance of these findings increases, the authors noted. Further research is needed, the authors added, to clarify the underlying biological mechanism for the association between depression and complications of diabetes, and to test interventions which might be effective in lowering the risk of complications among patients who have both diabetes and depression.
In addition to Lin, the researchers on the study were Dr. Carolyn M. Rutter, Malia Oliver, Dr. Evette Ludman, Dr. David McCulloch and Dr. Michael Van Korff of the Group Health Research Institute in Seattle, Dr. Wayne Katon and Dr. Paul Ciechanowski, both of the UW Department of Psychiatry and Behavioral Sciences; Dr. Susan Heckbert of the Cardiovascular Research Unit, UW Department of Epidemiology; Dr. Bessie Young of the Epidemiologic Research Information Center at the Veterans Affairs Puget Sound Health Care System and the UW School of Medicine, and Dr. Lisa Williams of the Division of Dermatology, UW Department of Medicine.
Grants from the National Institutes of Health supported the research.