November 10, 2005
Studying ions to help hearts
A patient has a heart attack, and is rushed to the hospital for treatment. He is treated and released, seemingly fine.
But then, two days later, a second cardiac event strikes, and the man is in far worse shape than before. Physicians treating him find that he was affected by cardiac arrhythmia, or an irregular heartbeat.
Such a scenario happens occasionally with cardiac patients — one to two days after a myocardial infarction, or heart attack, a patient can be hit by a major arrhythmia that can stop his heart.
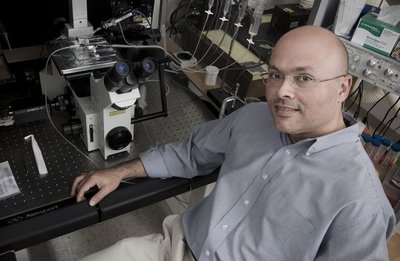
The secret to that irregular heartbeat lies in potassium and calcium ion channels, which control electrical impulses that drive the heart muscle. Dr. Luis Fernando Santana, an assistant professor of physiology and biophysics at the UW, studies those ion channels.
Santana and other researchers now know that post-heart attack arrhythmias strike because the heart’s electrical impulse system has gone drastically out of sync. In a normal heart, there is a balance between calcium and potassium ion levels in both the outer and inner walls of the heart. That balance keeps electrical energy flowing correctly through the heart, and allows the heart muscle to expand and contract as the heart beats.
But after a heart attack, the calcium ion levels in the heart can increase drastically, essentially reversing the balance of ion levels. That throws off the heart’s rhythm, to disastrous consequences — patients with severe cardiac arrhythmia shortly after a heart attack can die with little warning.
By looking more closely at those ion channels in the heart, Santana and his colleagues have pinpointed why ion levels are thrown out of balance after a heart attack — a cellular signaling pathway known as the calcineurin/NFAT transcriptional pathway. Following a heart attack, that signaling pathway is activated nearly five times more than normal. This results in a decrease in expression and function of potassium ion channels, which indirectly throw intracellular calcium ion levels out of balance, upsetting the rhythm of the heart.
Fortunately, beta blocker drugs, which are often prescribed after a heart attack, can suppress the pathway, staving off a potentially lethal cardiac arrhythmia.
As Santana has continued to study the calcineurin/NFAT transcriptional pathway, he has found that the very same pathway plays a role in controlling the action of vascular cells, which are found in arteries and veins. A similar calcium ion level imbalance in those cells can cause vascular walls to constrict steadily over time, leading to a constant buildup in blood pressure, for instance.
In fact, Santana hopes to show that the calcineurin/NFAT transcriptional pathway represents a calcium-driven signaling pathway that can be involved in modulating other processes in the body that involve electrical impulses.
“We think this could be a model for the fine-tuning of excitation in cells around the body, including neurons,” said Santana. “Because this pathway is self-sustained — an increase in calcium leads to changes in potassium function, which in turn increases calcium further — it could, for example, be part of a fundamental process for building memory at the cellular level.”
Santana will discuss his work on ion channels at a New Investigator Science in Medicine Lecture, from noon to 1 p.m. on Thursday, Nov. 17, in room T-625 of the UW Health Sciences Building.
After earning a bachelor’s degree in marine biology from the University of Puerto Rico, Santana went to the University of Maryland, where he completed his doctorate in physiology in 1996.
He joined the UW Department of Physiology and Biophysics in 2001 after postdoctoral work at the University of Maryland and the University of Vermont.