May 30, 2002
Pathway from stress to heart disease
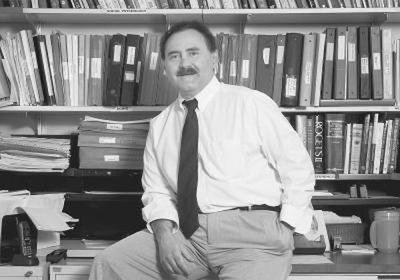
The well-known link between stress and heart disease starts with stress and other factors that can lead to poor health habits, according to a new UW study led by Dr. Peter Vitaliano, professor of psychiatry and behavioral sciences and of psychology.
Until now, little was known about exactly how chronic stress led to coronary heart disease, but the study published in the May issue of Psychosomatic Medicine sheds new light on the potentially deadly process.
Vitaliano reports that while the exact path connecting chronic stress and heart disease may vary from person to person, there appears to be a general pattern — at least in men.
First, chronic stress is associated with psychological distress; factors such as unsatisfactory social supports and poor coping skills may contribute to the link. The psychological distress is associated with poor health habits, such as insufficient exercise and poor diet, and a number of changes in body composition and metabolism that are well-established risk factors for heart disease. Eventually, these changes in body composition and chemistry — known collectively as the metabolic syndrome — produce heart disease.
Evidence for this model comes from a 30-month study of 152 married, older adults conducted by Vitaliano and his colleagues. Eighty of the subjects were caregivers for spouses with Alzheimer’s disease; previous studies have shown that such caregivers routinely experience numerous physical, emotional and financial stressors.
“The demands of caregiving, coupled with the biological vulnerabilities of aging, put spouse caregivers at increased risk for [coronary heart disease],” making them an ideal population for studying the relationship between heart disease and chronic stress, Vitaliano explains. The other 72 adults, none of them caregivers, served as a comparison group.
The researchers began by examining each subject for attributes that tend to produce psychological distress, such as low income, high exposure to stressors and insufficient coping skills. At the same time, they assessed each subject’s level of psychological distress, including depressive symptoms and sleep problems; obtained a self-rating of exercise and diet habits; and looked for indications of metabolic syndrome, including obesity, high blood pressure, and elevated blood levels of cholesterol, insulin and sugar. The researchers repeated all the evaluations 15 to 18 months later.
As expected, their findings revealed that the caregivers started from a more vulnerable position than the comparison group, with a greater tendency to suffer from such problems as obesity, depression, and disturbed sleep.
Heart disease was equally prevalent among the caregivers and comparison group when the study began. However, 27 to 30 months later, 54 percent of caregiver men suffered from heart disease, compared to only 26 percent of comparison group men.
Through a series of statistical analyses, the researchers were able to identify the most common path connecting stress to heart disease among the male caregivers. One of their strongest findings, Vitaliano points out, is that “in men, the pathway from [psychological] distress to the metabolic syndrome was one of the largest pathways from caregiving to [heart disease].”
His team’s findings suggest both a direct, immediate relationship between distress and metabolic syndrome, and an indirect, delayed link where distress promotes poor health habits that, over time, exacerbate metabolic syndrome.
Because hormone replacement therapy may affect many of the factors that predispose a woman to heart disease, the investigators broke the women into two groups: those using the therapy and those not using it. Evidence of a connection between chronic stress and heart disease was less clear in either group of women than it was among the men. However, the findings suggest that two different sequences of events link stress to heart disease in women who do and don’t take replacement hormones, and that neither sequence in women is the same as that in men.
Funding for the research was provided by grants from the National Institute of Mental Health, the National Institute on Aging, the National Cancer Institute and the National Heart, Lung, and Blood Institute.
Psychosomatic Medicine is the official bimonthly peer-reviewed journal of the American Psychosomatic Society. For information about the journal or to read the paper, visit